We all know at least one person who is taking medication for diabetes.
What we don’t know is that there is twice the number, since 1 in 2 (50%) people living with diabetes don’t know they have the disease.
You could be that other, yet-to-be-diagnosed diabetic.
Prolonged high blood sugar is unhealthy for the human body and may cause long-term, irreversible damage to organs in the body.
Glaucoma, the second-most common cause of blindness, has a direct link to long-term, uncontrolled high blood sugar (glucose).
Untreated diabetes is one of the most common risk factors for leg amputations and remains a leading cardiovascular disease risk factor and stroke risk factor.
It cannot be overemphasized; therefore, you need to monitor your blood sugar (blood glucose) level and control it.
Besides, early diagnosis and the commencement of lifestyle modification with or without drug treatment significantly slow down the progression of the disease.
What is diabetes mellitus?

Diabetes is a metabolic disorder in which blood sugar is high because of the body’s reduced ability or total inability to break down (metabolize) sugar (glucose).
In addition, protein and fat (lipids) breakdown (metabolism) are also affected.
To carry out this purpose of controlling blood sugar levels, the body depends on a hormone called insulin.
Insulin is a hormone produced by the pancreas, a sickle-shaped organ that is close to the liver and stomach.
Within the pancreas, a specialized group called beta cells produces insulin.
Certain conditions completely or partially destroy these pancreatic beta cells, thus crippling insulin production.
Diabetes, pancreatitis, or autoimmunity can destroy the beta cells.
Major Abnormalities in Diabetes
The two major abnormalities that occur to result in uncontrollably high blood glucose are:
- Insulin Deficiency: Insulin levels are reduced or absent.
- Insulin Resistance: Insulin levels are normal, but cells cannot interact with them.
When glucose is taken into the body, it must enter the cells, where it is broken down to give the body energy.
Insulin is required to carry most of the glucose into the cell.
In the absence of insulin, if the required amount is reduced or if the cells cannot recognize insulin, blood sugar will rise.
When this rise is sustained over a prolonged period, damage to organs in the body begins and is not reversible.
Values for Blood Sugar Levels
Blood sugar levels change but must fall within a defined range to be considered normal.
A fasting blood glucose (pre-prandial) shows the minimum expected range when an individual has been without food for at least 8 hours.
After a meal, blood glucose rises steeply.
When a 2-hour postprandial sugar level is measured, it must fall within a defined setpoint as well.
An individual is considered prediabetic when their blood sugar is above the normal range yet below the set point to be called diabetic.
Individuals in this category sooner or later develop full-blown diabetes.
The table below shows the corresponding values for which blood sugar is categorized:
| Fasting | 2 hours after a meal | Glycated Hemoglobin (HBA1C) | |
| Normal | 70–99 mg/dl
(3.9–5.5 mmol/L) |
Less than 140mg/dl
(7.8mmol/L) |
Less than 5.9% |
| Prediabetic | >100–125 mg/dl
(5.6–6.9 mmol/L) |
141–200 mg/dl
(7.8–11.1 mmol/L) |
6.0 -6.4% |
| Diabetic | Greater than 125mg/dl
(>6.9mmol/L) |
6.5% and above |
The table above shows ranges for blood sugar levels.
Fasting (pre-prandial), 2 hours after a meal (2 hours post-prandial).
HBA1C (glycated hemoglobin) is the concentration of glucose in red blood cells.
It is used as an indicator of blood sugar levels over some time (the last 3 months).
Types of diabetes mellitus
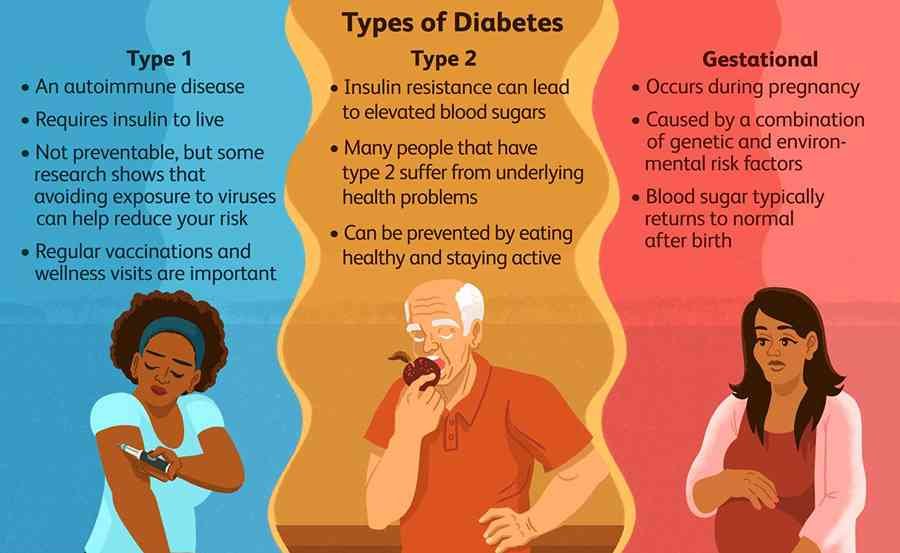
1. Type I diabetes
This accounts for 5–10% of diabetes; it is also called insulin-dependent diabetes.
There is autoimmune destruction of pancreatic beta cells, resulting in insulin deficiency.
Patients with this type of diabetes will depend on external insulin treatment for life, among other diabetic medications.
Type 1 diabetes often occurs at a young age.
2. Type II diabetes
This accounts for most diagnoses of diabetes (90–95%). usually seen in older individuals, although there has been a gradual shift, and this is diagnosed in the second decade of life.
It is also called insulin-independent as the primary abnormality is usually insulin resistance, although insulin deficiency subsequently occurs; thus, patients with type 2 diabetes later require external insulin therapy with other diabetic medications to survive.
3. Hyperglycemia first detected in pregnancy
This is the type of diabetes first seen in pregnancy in a mother who was previously not diabetic.
It is termed pregnancy-induced diabetes.
It often goes away after delivery
4. Others
- Unclassified
- Hybrid form
Risk factors for developing diabetes
Non-modifiable risk factors
- Age 45+
- Family history: if blood relatives have diabetes, your risk increases
- Race or ethnic background: Latino/Hispanic Americans, African Americans, Native Americans, or Pacific Islanders. Indians have a higher risk of developing diabetes at a younger age
Modifiable risk factors
- Overweight or obesity
- If your weight is 20% or more than your ideal body weight (losing 5 – 7% body weight reduces risk by half),
- Sedentary Lifestyle: Physical Inactivity
- High blood pressure
- Abnormal cholesterol levels
Symptoms and signs of diabetes

- Often Asymptomatic
- Increased urination (polyuria)
- Increased thirst (polydipsia)
- Increased food intake (polyphagia)
- Weight loss
- Body weakness
- Blurred vision
- Frequent body surface infections (vaginitis, fungal skin infections)
- Slow wound healing
Making a diagnosis of diabetes

Your doctor may request a simple blood test if you present with symptoms or signs, have risk factors, or have a routine medical check-up.
Usually, a finger prick is made with a needle and a drop of blood smeared on a hand-held instrument called the glucometer.
Approaches for Diagnosis
- One-step Approach: This is done using the HBA1C, or Oral Glucose Tolerance Test (OGTT): An individual is given a glucose meal and the blood sugar is measured after 2 hours
- Two-step Approach
- The value obtained is called the random blood sugar or glucose (RBS/RBG). If the value is high, a second test is done: fasting blood sugar or fasting blood glucose (FBS or FBG).
- Other tests may be requested to aid the diagnostic workup if test results show diabetes. These include fasting lipid profile, urea electrolyte, and creatinine; fundoscopy if there is difficulty weeing with the eyes; a Doppler ultrasound scan if there are leg problems; a wound swab MCS if there are non-healing wounds on the body; and a pancreatic beta-cell function test; however, this is reserved for long-term diabetics, type 1 diabetics, and patients with a low body mass index.
The table below shows the diagnostic values for diabetes:
| Normal | Prediabetes | Diabetes | |
| Random | Below 200 mg/dl, 11.1mmol/L | N/A | 200mg/dl or more
11.1mmol/L or more |
| Fasting | Below 100mg/dl
5.5mmol/L |
100–125 mg/dl
5.5–6.9 mmol/L |
126mg/dl or more
7.0 mmol/L or more |
| 2 hours Post-prandial | Below 140mg/dl
7.8mmol/L |
140–199 mg/dl
7.8–11.0 mmol/L |
200mg/dl or more
11.1mmol/L or more |
| HBA1C | Less than 5.9% | 6.0 – 6.4% | 6.5% and more |
Prevention/treatment
Type 2 diabetes and gestational diabetes can be prevented by lifestyle changes.
Increasing physical activity (exercise), moderate intake of carbs, and a high-fat diet—fruits, vegetables, and nuts—should make up a significant part of your diet.
These would help you maintain a healthy body weight.
You should regularly monitor your blood pressure, and if hypertensive, you should commence and stay adherent to the treatment prescribed by your doctor.
You should regularly monitor your blood sugar, at least 2 to 3 times a year.
Once your sugar control is impaired (pre-diabetic) or it shows that you have diabetes, your doctor will commence dietary control as mentioned above, with or without drugs.
If the diabetes is established to be type 1, you will be started on insulin with other hypoglycemic agents.
Complications
The complications of diabetes are what makes it a very dangerous disease.
It affects every organ and system in the body.
Below are some of the complications of diabetes:
- Stroke
- visual impairment/blindness
- Heart damage
- infertility
- The poor wound-healing ability
- Difficult labor due to fetal macrosomia( larger than normal babies)
- Leg ulcers
- skin, muscle, and bone infections
- Kidney damage
- weakened immune system, hence the poor ability of the body to fight disease
- Atherosclerosis is the thickening of blood vessels, which will ultimately increase blood pressure.
- Increased rate of clot formation (hypercoagulability)
- Poor covid-19 outcome
Conclusion
Diabetes is one of the most common diseases around, yet it is still underdiagnosed.
Most people live with diabetes unknowingly and are often present in the hospital when complications have set in.
If you are not knowledgeable about your blood glucose level, check in with your GP, get tested and, where applicable, commence treatment.
However, there are a lot of lifestyle choices that you can make today to significantly reduce your risk of coming down with the disease.
Dr. Choji Choji
Medical professional with a Bachelor of Medicine, Bachelor of Surgery (MBBS) from University of Jos. Has special interest in writing and public health education. Beliefs strongly that adequate patient-information is key to compliance with care.