Glucose-6-phosphate dehydrogenase (G6PD) is an enzyme (a type of protein important for cell function) involved in energy production.
It is present in all cells, including red blood cells, and protects them from certain toxic by-products of cellular metabolism.
In people with G6PD deficiency, red blood cells do not produce enough G6PD or do not work as they should, and without enough G6PD to protect them, red blood cells break down under certain conditions (Hemolysis).
Genetic basis of G6PD
G6PD deficiency is a genetic disease.
When a person who inherits this disease is exposed to irritants (such as a cold, infections, certain drugs, or other substances), the regulation of the outer layer of red blood cells (skin cells) changes significantly.
G6PD also protects the RBCs from potentially harmful by-products that can come from fighting infections or certain medications.
The G6PD test is a simple test that requires a blood test.
This test measures the level of glucose-6-phosphate dehydrogenase (G6PD) in red blood cells to diagnose deficiency.
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is a more common genetic condition in men of African heritage.
It is also commonly found in people from the Mediterranean and Southeast Asia, meaning they are more likely to infect men than women, making them more susceptible to infections.
They pass the gene on to their offspring, but they (parents) show no symptoms (asymptomatic).
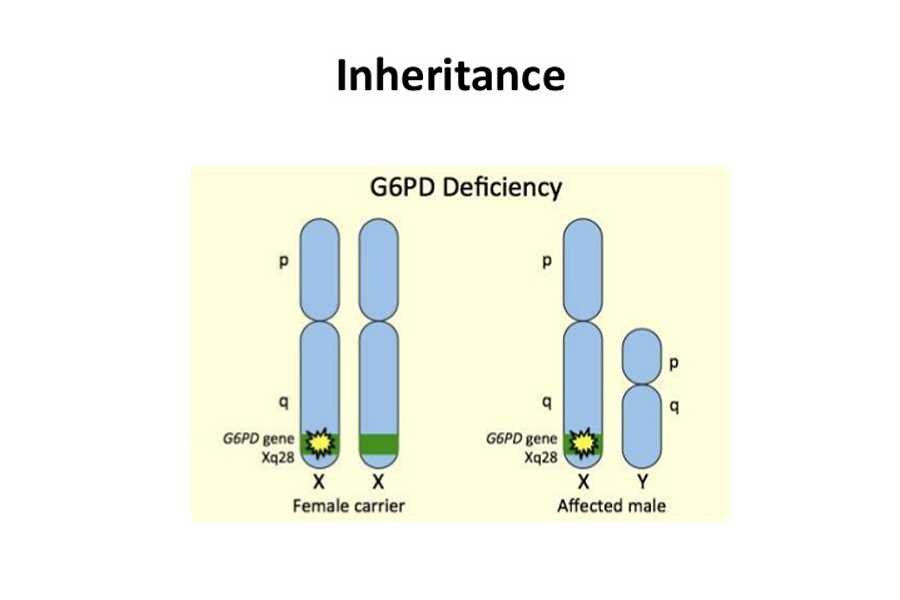
The gene responsible for this is found on the X chromosome.
The physical diagnosis of patients with G6PD may be normal, but not in all cases.
The deficiency can lead to anemia called hemolytic anemia.
Certain foods, medications, infections, and severe stress can cause hemolysis.
A hemolytic event is the rapid destruction of red blood cells.
In patients with hemolytic anemia, the body cannot produce enough red blood cells to replace the destroyed red blood cells.
The G6PD test is typically used to diagnose the cause of hemolytic anemia.
What are the reasons your doctor might request the G6PD assay?
Physicians may decide that their patients undergo G6PD tests if they suspect hemolytic anemia based on the following symptoms:
- Paleness
- An enlarged Spleen and Liver
- Jaundice
- Shortness of breath
- Increased heart rate
- Extreme Tiredness
- Dark-coloured urine
What should you do before the test?
Some medications can affect the results of these tests.
Inform your healthcare provider what medications you are taking, including prescription drugs and supplements.
He or she will advise you to stop taking it or not before the G6PD test is carried out, as this can alter the result of the test.
The tests should not be done immediately after a blood transfusion, and you should provide your doctor with your health history before you are diagnosed with G6PD.
Your healthcare provider should take note of the area you originate from, whether it is from a place where the condition is common, if you have a family history of G6PD, or if you are living with an unknown form of anemia.
All of this can negate your result if not taken into consideration before the test is carried out.
Avoid chemical substances like naphthalene.
Let your doctor know if you’ve recently eaten Fava Beans or taken Sulfonamide Drugs (Sulfonamide drugs kill bacteria and fungi by interfering with their metabolism).
Sulfonamide drugs can cause adverse reactions, especially in people with G6PD deficiencies.
Sulfonamide drugs may include:
- Anticonvulsants
- Antibacterial drugs
- Antifungal drugs
How is the test done?
G6PD deficiency can be diagnosed by performing a blood test to check the G6PD enzyme level in the blood, and this can be done by withdrawing the blood sample from a qualified technician, nurse, or healthcare provider in a hospital diagnostic center or laboratory.
The preferred site on your skin for the withdrawal will be cleaned with gauze soaked in methylated spirit or antiseptics to prevent contamination of the site by microorganisms.
Tunicate will be wrapped to apply pressure to the site, as this will help make the veins more visible and accessible through a sterilized needle and syringe.
The technician will patiently insert the needle into the venipuncture site, withdraw blood of up to 5 ml, and patiently dispense the blood withdrawn into a LAVENDER (EDTA), GREEN-TOP (HEPARIN) tube and send it in for laboratory testing.
Apply gauze to the venipuncture site to stop bleeding from the site.
What should you do after the test?
The result of the test should be discussed at an agreed-upon later date of appointment with the doctor.
There are some triggers you should avoid, as they can trigger a quick loss of red blood cells over a short period of time.
If the result states a low glucose-6-phosphate dehydrogenase enzyme level in the blood, this indicates that there is a deficiency.
Whereas a normal test result that indicates NO G6PD for an adult ranges from 5.5 to 20.5 units/hemoglobin.
There are other things you should avoid because they could cause complications.
These substances include:
- Antimalarial drugs (quinine)
- Quercetin (the ingredient in some dietary supplements)
- Nitrofurantoin (a drug used to treat urinary tract infections)
- Aspirin and nonsteroidal anti-inflammatory drugs.
Possible test outcomes
The reference range for normal G6PD activity is 10.15–14.71 U/g Hb for neonates and 6.75–11.95 U/g Hb for adults.
Any result coming out of those ranges is abnormal.
On the other hand, the test is known as the G6PD screen or the RBC G6PD test.
In severe cases, it can also lead to kidney failure or death.
Fortunately, the symptoms of G6PD deficiency often disappear after the trigger has been confirmed and removed.
When the condition is diagnosed and treated appropriately, children with G6PD deficiency can live healthily.
Interpretation of test result
Normal levels of the G6PD enzyme in a male indicate that it is unlikely to be deficient, and if there is anemia, it is likely to be due to another cause.
However, if the test was performed during an episode of hemolytic anemia, it should be repeated a few weeks later, when the RBC population is overcrowded and mature.
When the enzyme glucose-6-phosphate dehydrogenase exhibits low levels in the blood, this reflects a deficiency.
The patient may have symptoms when they are exposed to triggers like stress, chemicals, and some medications.
The result, however, is not enough to predict how the patient will react in some circumstances.
Serious symptoms vary from person to person and from episode to episode.
G6PD cannot be transferred from one person to another.
G6PD deficiency cannot be cured, and it is a lifelong condition.
However, most people with G6PD deficiency live completely normal lives as long as they avoid the causes.
Conclusion
Detecting an enzyme deficiency allows people to work with their doctor and be trained for a condition that will affect them somewhat throughout their lives.
It also allows people to talk to their healthcare provider about how this trait is inherited and the potential impact it can have on their children.
Knowing about the disability and avoiding potential substances and the causes of disease, most people with G6PD deficiency can lead a relatively normal life.
Treating the symptoms of G6PD deficiency is usually as simple as removing the trigger.
This often means treating the infection or stopping the medication.
A child with severe anemia may need hospital treatment to get oxygen and fluids.
Sometimes babies also need a transfusion of healthy blood cells.
The most important aspect of managing G6PD deficiency is avoiding the means that could trigger an attack.
In cases of acute hemolytic anemia, a blood transfusion or even a blood transfusion may be needed.
Oke-Adedayo Isreal
A Public Health Specialist, an advocate and a social development worker who loves to make positive impact most especially on issues relating to health and population development. A highly resourceful, flexible, innovative, team player and an enthusiastic individual who possesses considerable amount of knowledge regarding epidemiology, monitoring and evaluation, environmental and occupational health.



