Pulmonary embolism (PE) is a life-threatening medical emergency that often lurks in the shadows, requiring prompt recognition and intervention.
This can disrupt the blood flow and oxygen delivery to your tissues, potentially leading to life-threatening complications.
This blog post aims to shed light on this critical condition, providing insights into its causes, symptoms, diagnosis, and management.
Let’s delve into the world of pulmonary embolism and unravel the complexities surrounding this silent threat.
Pulmonary embolism
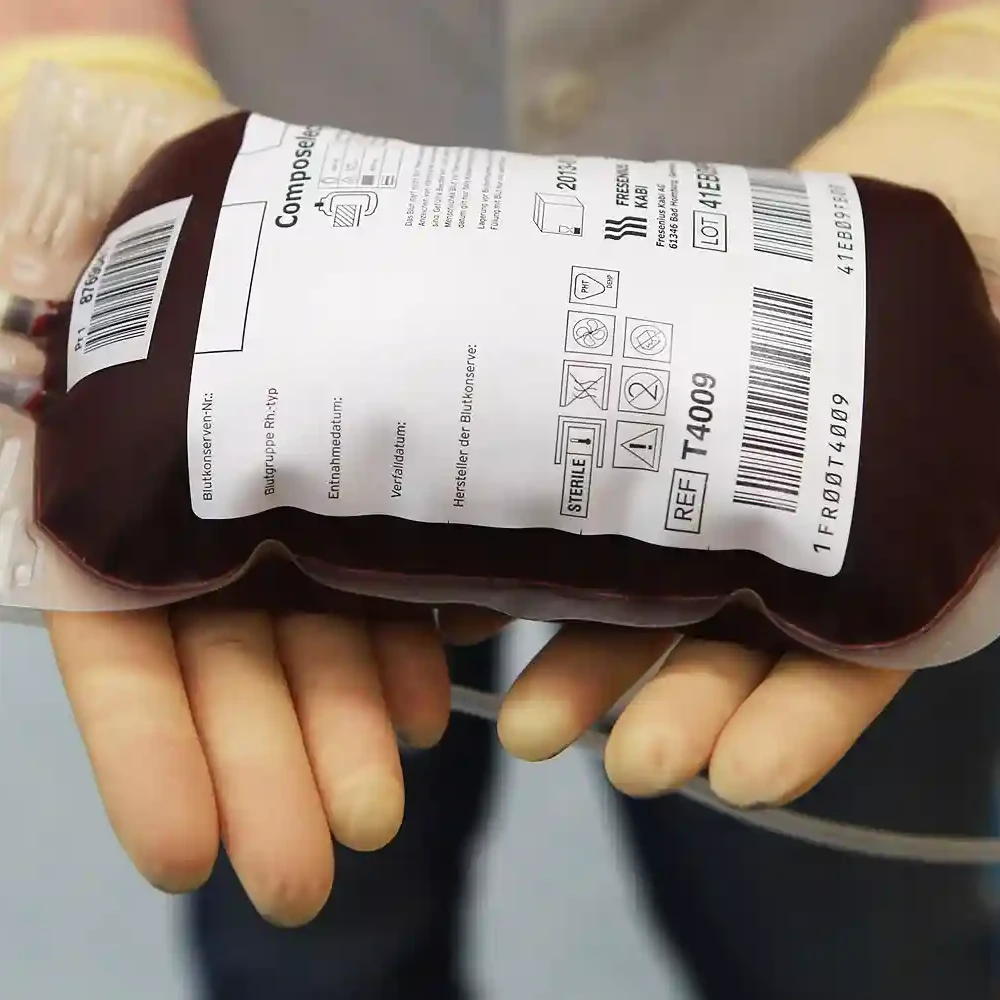
Blood clots are essentially clumps of blood cells that stick together.
While they’re sometimes necessary to heal wounds, they can also form in the wrong places, causing problems like PE.
Pulmonary embolism occurs when a blood clot, usually originating in the deep veins of the legs (deep vein thrombosis, DVT), travels through the bloodstream and lodges in the pulmonary arteries, obstructing blood flow to the lungs.
This sudden blockage can have severe consequences, ranging from respiratory problems and distress to cardiac compromise.
Risk factors for pulmonary embolism
Understanding the risk factors for pulmonary embolism is crucial for prevention.
Common predisposing factors include:
- Immobility: prolonged bed rest or long flights.
- Surgery: especially orthopedic procedures, in the legs and pelvis
- Cancer: increased clotting risk.
- Pregnancy: as well as having a recent childbirth
- Smoking and obesity: lifestyle factors that contribute to vascular complications.
- Prior History: Individuals with a history of DVT or PE are at increased risk.
- Hormone therapy: such as birth control pills or estrogen replacement therapy
Recognizing the signs and symptoms
Identifying the signs and symptoms of pulmonary embolism is crucial for early intervention.
While the presentation can vary, common indicators include:
- Shortness of breath: sudden and unexplained.
- Chest pain: often sharp and exacerbated by deep breaths or coughing.
- Rapid heart rate: Tachycardia may indicate the heart’s effort to compensate for decreased oxygenation.
- Cough with or without blood: hemoptysis may occur in some cases.
- Leg swelling and pain: a potential sign of deep vein thrombosis (DVT).
If you experience any of these symptoms, it’s crucial to seek immediate medical attention.
Early diagnosis and treatment can significantly improve your chances of a full recovery.
Diagnostic approaches for pulmonary embolism
A timely and accurate diagnosis is paramount to managing pulmonary embolism effectively.
Common diagnostic tools include:
1. CT Pulmonary Angiography (CTPA)
A widely used imaging technique that provides detailed images of the pulmonary arteries to confirm or rule out pulmonary embolism.
Unlike conventional X-rays that capture flat images, CTPA scans employ rotating X-ray beams to generate detailed cross-sectional views of the body.
This allows for a meticulous examination of the intricate lung vasculature, pinpointing even small clots that might evade other imaging methods.
2. D-dimer Test
Measures a specific substance released when a blood clot breaks up.
Elevated levels may suggest the presence of clotting, but further diagnostic tests are necessary for confirmation.
3. Ventilation-Perfusion (V/Q) Scan
Utilized when a CT scan is contraindicated, this test evaluates airflow and blood flow in the lungs.
Prevention of pulmonary embolism
There are several steps you can take to reduce your risk of developing the disease.
- Maintain a healthy weight
- Get regular exercise
- Avoid prolonged sitting or immobility
- Anticoagulant therapy in high-risk situations
- Wear compression stockings after surgery or during long periods of sitting
- Talk to your doctor about your risk factors and preventive measures
Treatment options for pulmonary embolism
Management of pulmonary embolism involves stabilizing the patient and preventing further clot propagation. Key treatment modalities include:
- Immediate care: This can include the administration of oxygen for breathlessness, pain relievers for chest pain, etc.
- Anticoagulant Therapy: Heparin and subsequent transition to oral anticoagulants like warfarin or direct oral anticoagulants (DOACs).
- Thrombolytic Therapy: reserved for massive pulmonary embolism with hemodynamic instability.
- Inferior Vena Cava (IVC) Filters: Placement in cases where anticoagulation is contraindicated or ineffective.
Conclusion
Pulmonary embolism is a critical condition with potentially dire consequences.
Understanding its risk factors, recognizing symptoms, and employing timely diagnostic and therapeutic interventions are paramount to ensuring positive outcomes.
If you suspect pulmonary embolism or exhibit concerning symptoms, seek immediate medical attention.
It is essential to work collaboratively with healthcare professionals to tailor preventive strategies and manage this silent threat effectively.
Obisesan Damola
Damola is a medical doctor who has worked in the Nigerian healthcare industry for a little over 3 years in a number of primary, secondary, and tertiary hospitals. He is interested in and writes about how technology is helping to shape the healthcare industry. He graduated from the College of Medicine, University of Ibadan, the foremost medical training institution in Nigeria.