Telemedicine
Telemedicine is the use of virtual methods of providing medical care using digital devices such as computers and smartphones to patients from a remote location.
Commonly, telemedicine is done via video conferencing, phone calls, messages, emails, etc.
Telemedicine became prominent during the COVID-19 pandemic, when many states and countries were in lockdown, as patients with chronic diseases like diabetes and hypertension, had to consult with their doctors regularly.
Telemedicine offers a range of benefits for both patients and healthcare providers.
It is possible to access a wide range of care options through telemedicine services, including primary healthcare consultations, medication reviews, psychotherapy, counseling sessions, physical therapy, dental care, emergency treatment of asthma, etc.
Telemedicine is increasingly proving to be transformative, even in a large country where access to providers is limited.
Professionals in health and information technology believe that telemedicine will gain more popularity over the next few years.
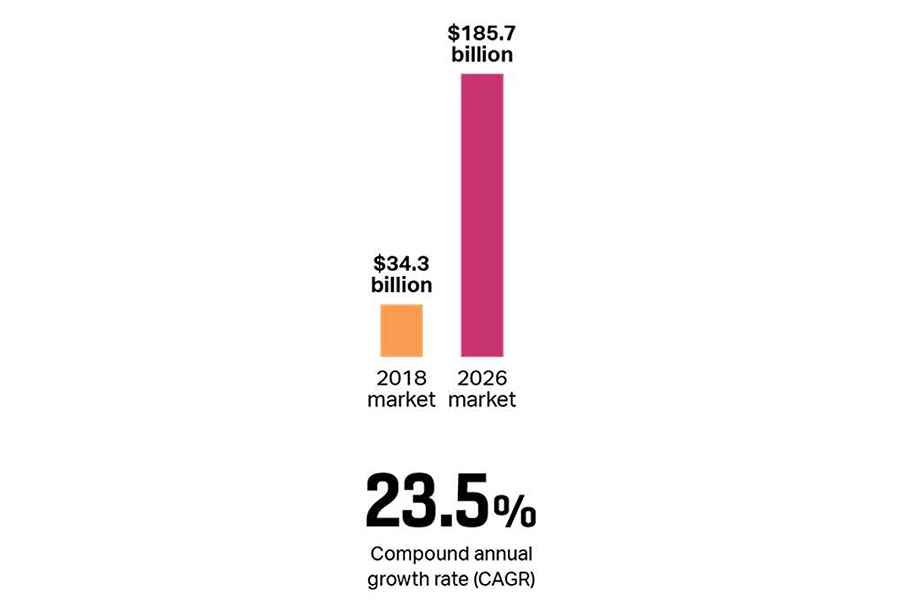
Research by Fortune Business Insights titled “TELEMEDICINE: GLOBAL MARKET ANALYSIS, INSIGHTS, AND FORECAST, 2019-2026″ revealed that on a global scale, the telemedicine market will flourish from the global market worth of US$ 34,289.2 million in 2018 to reach USD 185.66 billion by 2026 at a 23.5% CAGR.
Several factors have contributed to the growth of the telemedicine market, including increased traditional healthcare costs, a recent boost in funding for telemedicine, the COVID-19 pandemic, and an increase in users opting for digital healthcare.
Examples of telemedicine services in Nigeria include CribMD, Doctall, Doctorcare247, DoktorConnect, DRO Health, Health Connect 24/7, Hudibia, LaFiya Telehealth, Reliance HMO, and Tremendoc
Telehealth vs telemedicine
The terms telemedicine and telehealth bring with them several debates in usage among individuals in the healthcare field.
While some often use them interchangeably, there is, of course, a distinction between the two.
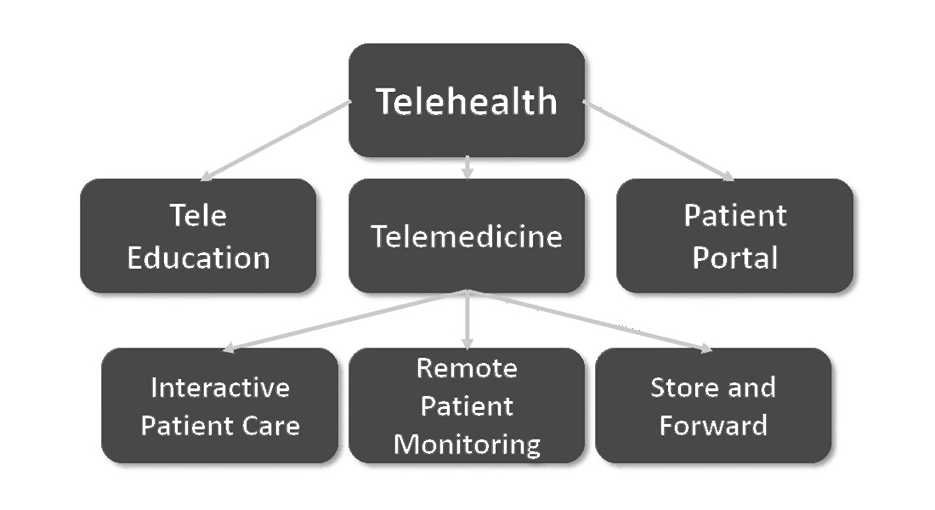
While telemedicine can be considered to be physician-focused, telehealth includes all remote interactions among health professionals in general.
Telehealth is the use of electronic information and telecommunications technologies to support and promote long-distance clinical health care, patient and professional health-related education, public health, and health administration – HealthIT
Telemedicine is the use of telecommunications and information technologies to provide remote clinical services to patients as well as physician-physician interactions concerning patients through the transmission of digital imaging, secure video and audio consultations, and remote medical diagnoses.
In contrast, telehealth is an umbrella body for telemedicine and non-clinical activities of health facilities, including physician training, administrative meetings, continuing medical education (CME), etc.
It is a collection of methods to improve patient care and health professional education.
Types of telemedicine
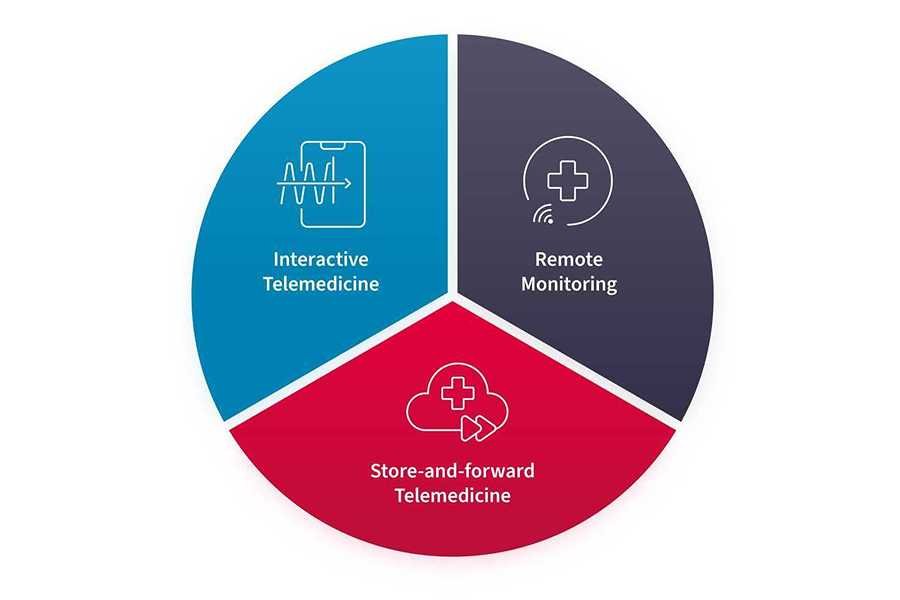
There are three main types of telemedicine, which include interactive medicine (patients and physicians communicate in real-time), remote patient monitoring (patients and/or their caregivers monitor their progress using mobile medical devices), and finally, store and forward (sharing of patient information between physicians remotely).
1. Interactive medicine or real-time telemedicine

Also known as interactive or real-time telemedicine, this allows patients and physicians to communicate virtually in real-time.
Methods employed include the use of mobile phones and tablets for consultations and video conferences.
Patient-physician interaction follows the patterns observed by face-to-face consultations, including taking a medical history, inquiry into presenting symptoms, and basic visual examinations.
This can also help offer immediate counseling to patients in emergencies that require prompt medical attention.
This is done while protecting the privacy of the patient and making sure their information is secure; hence, following appropriate data protection regulations, e.g., data encryption, and data sharing on a need-to-know basis.
2. Remote Patient Monitoring

This is also known as self-monitoring, self-testing, or telemonitoring.
Remote monitoring Telemedicine allows physicians to monitor their patients in their respective homes.
These solutions see extensive usage in the management of chronic conditions like hypertension and diabetes, as well as asthma.
They are important because they can transmit this data automatically to health personnel, who would keep an eye out for any signs of danger.
They help health professionals gain access to continuous patient health status data, making room for immediate intervention and boosting continuity of care.
Examples include sphygmomanometers (measure blood pressure), pulse oximeters (measure blood oxygen saturation), glucometers (measure blood glucose level), etc
3. Store and Forward

Store-and-forward telemedicine involves remote interactions between physicians and other health professionals concerning patient data and care.
This goes beyond remote patient-physician consultations to involve sharing patient information, e.g., radiographs, test results, etc., with other health professionals, usually specialists, who can provide more insight into patient care.
These solutions can transmit patient information across distances and systems, so the new professional can take off where the primary physician left off.
This gives patients access to a team of specialists from different parts of the world.
Worthy of note, these systems are designed to safeguard patient data with security features bearing in mind the patient’s privacy.
Benefits of telemedicine

1. Patients’ benefits
- Improved access to care as patients from anywhere on earth can gain access to health professionals from a remote location, especially the elderly and patients with mobility challenges.
- Preventive care is a big upside to the adoption of telemedicine, as physicians can watch out for patients with chronic health conditions in the comfort of their homes, offering real-time advice on their health status.
- Patients spend less time commuting and staying in the hospital, eliminating secondary spending and providing cost savings.
- Patients have shorter hospital stays as, when stable, they can be sent home and monitored remotely.
- Telemedicine boosts patient privacy by providing them with a secret virtual session with their physicians where they can share their information in a secluded environment.
- Telemedicine introduces convenience, as it allows people to access care in the comfort and privacy of their own homes.
- It eliminates the risk of contracting infections in a hospital or at the doctor’s office, thereby reducing the spread of these contagious nosocomial infections.
- Telemedicine solutions make use of readily available devices owned by the majority of patients, not requiring the procurement of separate gadgets.
- Remote care helps reduce patients’ time away from work
- Caregivers and family connections can stay in the loop about patient health status, irrespective of their location, by joining virtual consultations.
2. Benefits for healthcare providers
- Telemedicine helps increase revenue for health facilities and physicians, as they can care for more patients and make more money to supplement their basic income.
- These solutions make use of readily available devices to communicate with patients in a secure environment.
- The safety of physicians is ensured by virtual consultations, as they are not routinely exposed to patient diseases.
- With store and forward telemedicine, it is much easier to forward patient data to health specialists to collaborate on patient care.
- Telemedicine eases the management of chronic medical conditions that require frequent clinic visits, as these visits can be adequately observed virtually.
- Being able to access care from home without the hassle of commuting to the hospital increases patients’ satisfaction with the services of their healthcare provider.
- Health facilities experience lower admission rates as some patient groups can be monitored from home.
- Telemedicine is a way forward in the business world; it provides a competitive advantage for health facilities over other practices.
- Health facilities can increase their patient base by involving patients in remote places, thereby increasing their client base.
- Virtual consultations make room for assessing patients to see whether or not they need treatment in person.
- Telemedicine helps provide certain kinds of care, common mental health treatments, and the management of minor health conditions.
- Physicians can remotely access patient real-time data and hence review or renew patient prescriptions if need be.
- Offer certain types of therapy, such as speech therapy, that can be exclusively observed online.
- Facilities experience fewer missed appointments and reduced consultation cancellations since patients can access care at home.
Challenges to the adoption of telemedicine

However, telemedicine may not suit every person or situation.
There are some potential disadvantages to using telemedicine over traditional care methods.
The following sections look at some disadvantages for patients and healthcare providers.
Telemedicine is not a good fit for all patients.
Some drawbacks of this type of care include:
1. Patient-related
- Cost of service: remote care can be expensive to opt for as patients have to pay physician fees, buy internet data, and sometimes opt for software subscriptions to access care, thereby marginalizing poor patients from accessing remote care.
- Insurance coverage: Not all health insurance companies cover the use of telemedicine. Some users would have to pay for the service out of their pockets.
- Technology adoption: telemedicine is highly dependent on technology; a lack or low adoption of these technologies by a group of people, e.g., the elderly, would impact its use among them.
- Lack of technical know-how: patients must familiarise themselves with the software employed by their health providers or find themselves unable to access the needed care. are often limited by their lack of knowledge of how to operate normal or simple computer systems.
- Technical Error: technology is susceptible to errors and failures, including software incompatibility, network unavailability, server downtimes, etc For an important industry like the healthcare sector, this can be serious and, at times, life-threatening.
- Patient data security: health data is a major target for hackers. Despite advancements in data security, some users can still fall prey to these criminals, especially if the telemedicine channel is not encrypted.
2. Health providers related
- Data protection regulations: health providers have to follow very stringent data regulations to adopt telemedicine, which can slow down adoption.
- Professional licensing: physicians are not allowed to practice medicine outside of their licensing country or area; hence, they are not legally able to help patients who live outside of their licensing jurisdiction.
- Expensive technology: the cost of adoption can be a concern for health providers as it would impose a large cost at initiation, and there might be a subscription to pay for after some period. Transferring the added cost to patients might make providers lose them as well.
- Interoperability: Not all telemedicine solutions are designed to work with common electronic health records hence, health data silos could develop.
- Patient data security: health providers have to take extra measures to secure patient data by deploying advanced security measures, a measure not needed for traditional physical consultations.
- Challenges with physical examination: consultation time is increased with telemedicine; physicians can only rely on patient history, self-reported examination, and visual inspection of patients to make assessments of their conditions.
- Misdiagnosis: not being physically present for adequate assessment, patient conditions can be misdiagnosed, as not all illnesses can be diagnosed remotely.
- Reimbursement: getting paid for services can be an issue for providers, especially concerning patients with insurance coverage, as these insurance companies might not be ready to pay enough for their client base.
The future of telemedicine

Telemedicine provides the healthcare industry with many benefits, and its utilization will continue far into the future.
It was the saving grace during the pandemic, and what is clear is that it is here to stay.
Bearing this in mind, telemedicine solutions need to address pitfalls to their adoption to deliver the best health outcomes for patients.
Future projections in telemedicine include…
- Health data regulations: as telemedicine gains more ground and authorities become cognizant of its affairs, they will work on regulations and data policies to protect patient data and privacy appropriately, as well as enforce the incorporation of advanced security measures into telemedicine platforms.
- Across-border care: international relations might come up with a policy to allow specialists to practice remote care in regions where they have yet to be licensed to do so. This ensures patients can access specialists from anywhere around the world for care.
- Wearables: remote monitoring of patients would pave the way for the adoption of wearable technology as a means for physicians to access real-time patient data. make assessments of them and give recommendations. These wearables would also be incorporated into electronic health records to keep data in one place, avoiding silos.
- Collaborations in health platforms: interoperability would increase as organizations develop systems with data structures compatible with others or that follow a compatible, standardized structure. This ensures the ability to compatibly share patient data when needed and reduces data silos.
- Business and revenue growth with adoption: as with every industry that has adopted technology in its operations, healthcare would also experience business growth as the wide adoption of telemedicine would smooth patient care and the day-to-day operation of health facilities. Also, these facilities benefit financially from an increase in their patient base.
- Business funding: telemedicine will not be possible without the technological infrastructure to support it. Remote care would be attractive to investors as a fertile ground to build wealth, being a frontier in the future of healthcare. The field is expected to see a lot of backing from investors as founders try to come up with solutions that give patients the best experience.
- Fast access to specialists: telemedicine would give room for specialist centers where patients and other physicians can access specialists 24/7, unlike what is currently available, where patients wait weeks to be reviewed by specialists.
- Preference for telemedicine access: as more and more patients become cognizant of the impact of telemedicine, they get to adopt it as an alternative to conventional consultations. It would seek to choose facilities that offer telemedicine features for care.
- Reduced patient load and wait time in clinics: by widely adopting telemedicine, many patients would opt for remote consultations from their homes, leaving those with serious cases or requiring physical assessment, usually the minority, to visit clinics for care.
- Improved patient experience: an important factor in the adoption of technology is the user experience; the same applies to healthcare solutions. Patients want a seamless, easy-to-use, and integrated solution and not to juggle between three or more platforms to pay for care, request a physician, access their health records, etc. Facilities would opt for a one-in-all solution for their telemedicine platform where patients can do all they need to access care.
Obisesan Damola
Damola is a medical doctor who has worked in the Nigerian healthcare industry for a little over 3 years in a number of primary, secondary, and tertiary hospitals. He is interested in and writes about how technology is helping to shape the healthcare industry. He graduated from the College of Medicine, University of Ibadan, the foremost medical training institution in Nigeria.



