Healthcare is a dynamic and multifaceted domain that encompasses a vast array of services, professionals, and systems dedicated to promoting and maintaining the well-being of individuals and communities.
In this blog post, we will embark on a journey through what healthcare is, unraveling its pillars, exploring its diverse principles and spectrum, highlighting prevalent challenges, and shedding light on modern trends shaping the future of this critical field.
What is healthcare?
Healthcare is a human endeavor orchestrated to safeguard and enhance the well-being of individuals and communities.
It is a comprehensive system encompassing a wide array of services and interventions designed to promote, maintain, and restore health.
The main principles of healthcare are to prevent, diagnose, treat, and manage illnesses or conditions, as well as promote overall well-being.
Preventive care guides individuals and communities towards healthy lifestyles, fostering a culture of awareness and proactive measures like vaccinations and regular check-ups; diagnosis meticulously analyzes symptoms and gathers data, weaving a tapestry of clues to identify the origins of discord within the body; treatment employs an arsenal of interventions, from medication to surgery, to restore harmony and quell the disharmony of illness; and finally, rehabilitation helps individuals regain lost function and reintegrate into life’s vibrant tapestry after the storm of illness has passed.
Healthcare involves a network of healthcare professionals, institutions, and technologies working collaboratively to address the diverse needs of individuals and communities.
It extends beyond clinical settings, acknowledging the influence of social, environmental, and behavioral factors on health.
The goal is to not only treat illnesses but also to emphasize preventive care, patient education, and the overall well-being of individuals.
The pillars of healthcare
Healthcare, as a multifaceted system, stands on robust pillars that collectively support the well-being of individuals and communities.
These pillars form the foundational principles guiding the delivery of medical services, emphasizing accessibility, quality, and affordability.
In this essay, we will explore the pillars of healthcare, understanding their significance in shaping a resilient and effective healthcare system.
1. Accessibility
The pillar of accessibility is fundamental to healthcare, embodying the principle that essential medical services should be within reach of all individuals, regardless of socio-economic status, geographic location, or demographic characteristics.
Accessible healthcare ensures that no one is left behind, emphasizing the need for equitable distribution of healthcare facilities, professionals, and resources.
The creation of a healthcare system where individuals can readily seek and receive medical attention promotes preventive care, early diagnosis, and timely interventions.
Initiatives to address healthcare deserts, improve transportation infrastructure, and enhance telehealth services contribute to bolstering the accessibility pillar, creating a healthcare landscape that is inclusive and responsive to the diverse needs of populations.
2. Quality
Quality stands as an unwavering pillar, representing the commitment to delivering medical services that are safe, effective, and patient-centered.
The pursuit of quality in healthcare involves the integration of evidence-based practices, continuous improvement, and a focus on the overall patient experience.
Healthcare professionals play a pivotal role in upholding the quality pillar, ensuring accurate diagnosis, appropriate treatment, and compassionate care.
Robust health information systems, including electronic health records and data analytics, further support quality by facilitating informed decision-making and enabling coordinated care.
Embracing a culture of continuous learning, adherence to clinical guidelines, and patient safety initiatives all contribute to fortifying the quality pillar and fostering trust and confidence in healthcare delivery.
3. Affordability
Affordability stands as the pillar that addresses the financial dimensions of healthcare, recognizing that financial barriers should not impede individuals from seeking necessary medical care.
Healthcare financing models, public policies, and insurance mechanisms all play roles in ensuring that the cost of healthcare services remains manageable for individuals and communities.
Striking a balance between the need for sustainable financing and preventing financial hardship due to medical expenses is central to the affordability pillar.
Innovations in healthcare financing, including universal health coverage initiatives and community-based health insurance programs, contribute to building a healthcare system where financial considerations do not compromise access to essential medical services.
Principles of healthcare
Healthcare, as a fundamental societal pillar, operates on a set of principles aimed at promoting well-being, preventing illness, providing accurate diagnosis, delivering effective treatment, and supporting rehabilitation.
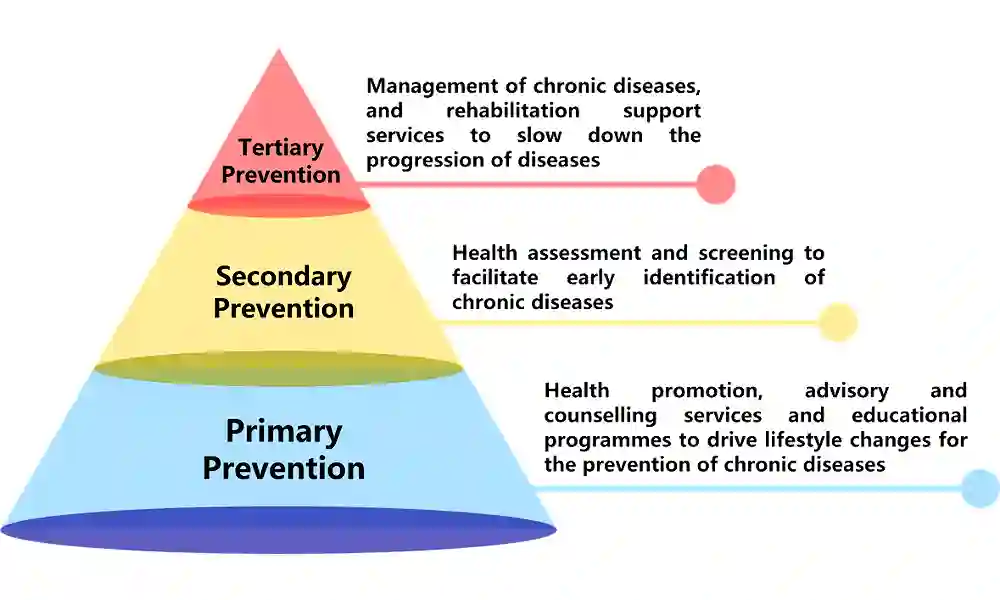
1. Prevention
Prevention in healthcare involves proactive measures aimed at avoiding the onset or progression of diseases and promoting overall health.
- Primary prevention: focused on preventing the occurrence of diseases through lifestyle interventions, immunizations, and health education.
- Secondary prevention: early detection and intervention to halt or slow the progression of diseases, often through screening and regular check-ups.
- Tertiary prevention: managing and minimizing the impact of existing conditions to prevent complications and disability.
Prevention is foundational to healthcare, as it not only reduces the burden of disease but also contributes to healthier communities and more sustainable healthcare systems.
2. Diagnosis
Diagnosis is the process of identifying the nature and cause of a disease or condition through clinical evaluation, tests, and examinations.
- Clinical assessment: gathering patient history, conducting physical examinations, and evaluating symptoms.
- Diagnostic tests: Utilizing laboratory tests, imaging studies, and other diagnostic procedures to confirm or rule out specific conditions.
- Collaboration: involving multidisciplinary teams and leveraging technology for accurate and timely diagnoses.
Accurate diagnosis forms the basis for effective treatment and rehabilitation, guiding healthcare professionals in tailoring interventions to address specific health issues.
3. Treatment
Treatment encompasses medical interventions, therapies, and strategies designed to address and manage health conditions following a precise diagnosis.
- Medication: the prescription of pharmacological agents to alleviate symptoms or address the root cause of a condition.
- Therapies: physical therapy, occupational therapy, and other rehabilitative interventions to enhance function and quality of life.
- Surgical interventions: invasive procedures performed to correct, repair, or remove damaged tissues or organs.
Effective treatment not only aims at curing diseases but also at improving the overall well-being of individuals, restoring function, and preventing complications.
4. Rehabilitation
Rehabilitation involves a structured and multidisciplinary approach to restoring physical, mental, and social well-being following illness or injury.
- Physical rehabilitation: exercise programs, mobility training, and activities to regain physical function.
- Occupational rehabilitation: strategies to enhance daily living skills and occupational functioning.
- Psychosocial support: counseling, mental health services, and community reintegration for holistic recovery.
Rehabilitation completes the healthcare continuum by fostering recovery, promoting independence, and maximizing the quality of life for individuals affected by illness or injury.
Spectrum of healthcare
Healthcare encompasses a spectrum of services aimed at promoting well-being, preventing illness, and treating various medical conditions.
Understanding the different types of healthcare is essential for individuals seeking appropriate and timely medical attention.
1. Primary healthcare
Primary healthcare is the first point of contact individuals have with the healthcare system.
It focuses on promoting overall health, preventing diseases, and addressing common health concerns.
Key features
- Services are provided by primary care physicians, nurse practitioners, and community health workers.
- Emphasis on preventive care, routine check-ups, vaccinations, and health education.
- Management of common illnesses and coordination of patient care.
Primary healthcare serves as the cornerstone of a well-functioning healthcare system, promoting health maintenance and early intervention to prevent the progression of illnesses.
2. Secondary healthcare
Secondary healthcare involves specialized medical services provided by healthcare professionals with advanced training and expertise.
It often requires a referral from primary care.
Key features
- Specialized medical practitioners include cardiologists, dermatologists, and orthopedic surgeons.
- Diagnostic services such as imaging, laboratory tests, and specialized medical procedures.
- Treatment and management of specific health conditions.
Secondary healthcare is crucial for diagnosing and managing complex medical conditions that may require specialized knowledge and advanced medical interventions.
3. Tertiary healthcare
Tertiary healthcare provides highly specialized and advanced medical care, often involving complex interventions, surgeries, and specialized treatment modalities.
Key features
- Tertiary care is typically provided in hospitals with advanced medical facilities.
- It involves specialized surgeries, organ transplants, and treatments for rare or severe medical conditions.
- Access to cutting-edge medical technologies and specialized medical teams.
Tertiary healthcare plays a critical role in managing severe and complex health conditions, offering advanced treatments that may not be available in other healthcare settings.
4. Quaternary healthcare
Quaternary healthcare involves highly specialized and experimental medical treatments, often associated with research institutions and academic medical centers.
Key features
- Focuses on innovative medical research, clinical trials, and experimental treatments.
- Provides care for patients with rare or extremely complex medical conditions.
- It involves collaboration between clinicians and researchers to push the boundaries of medical knowledge and treatment.
Quaternary healthcare explores new frontiers in medicine, contributing to advancements in medical science and offering potential breakthroughs for challenging health conditions.
5. Palliative and hospice care
Palliative and hospice care focuses on providing comfort, pain management, and emotional support for individuals facing serious, life-limiting illnesses.
Key features
- It is aimed at improving the quality of life for individuals with terminal illnesses.
- Addresses the physical, emotional, and spiritual aspects of end-of-life care.
- May include pain management, counseling, and support for patients and their families.
Palliative and hospice care play a vital role in ensuring dignity, comfort, and emotional support for individuals facing terminal illnesses and their families.
The components of healthcare
Healthcare, as a vital societal institution, is a complex and interconnected system comprising various components that work synergistically to provide medical services, promote preventive care, and enhance the overall well-being of individuals.
In this essay, we will delve into the intricate components of healthcare, examining the critical elements that collectively contribute to the functionality and success of healthcare systems.
1. Healthcare infrastructure
At the heart of healthcare is its infrastructure, which encompasses a network of facilities and institutions designed to provide medical services.
Hospitals, clinics, primary care centers, and specialty healthcare institutions form the physical backbone of healthcare infrastructure.
The distribution, accessibility, and quality of these facilities influence the overall reach of healthcare services within a population, playing a pivotal role in shaping the health outcomes of communities.
2. Healthcare professionals
The human capital of healthcare, comprised of skilled professionals, is an indispensable component that brings medical expertise, care, and compassion to patients.
This diverse group includes doctors, nurses, pharmacists, therapists, and various allied health professionals.
The competence, dedication, and collaboration of healthcare professionals are fundamental to effective patient care, diagnosis, treatment, and the overall functioning of healthcare systems.
3. Health information systems
The integration of health information systems is essential for the efficient management of patient information, supporting clinical decision-making, and contributing to public health initiatives.
Electronic health records (EHRs), data analytics, and health information exchanges form the data backbone of healthcare.
These systems facilitate the collection, storage, and analysis of health-related information, enabling healthcare providers to deliver evidence-based care and make informed decisions.
4. Governance and policy
Effective governance and policies provide the regulatory framework within which healthcare systems operate.
Governments, health authorities, and regulatory bodies play a crucial role in shaping the direction of healthcare, ensuring adherence to ethical standards, licensing healthcare providers, and formulating policies that address public health challenges.
Strong governance fosters accountability, transparency, and responsiveness to the evolving needs of populations.
Challenges in healthcare
- Access disparities: Disparities in access to healthcare services persist, influenced by socio-economic factors, geographic location, and demographic characteristics. Addressing these disparities requires targeted interventions and policy initiatives aimed at improving accessibility for marginalized populations.
- Workforce shortages: Many regions face shortages in specific healthcare professions, leading to challenges in meeting the growing demand for medical services. Opportunities lie in investing in education and training programs to address these shortages and diversify the healthcare workforce.
- Interprofessional collaboration: Enhancing collaboration among different members of the healthcare cadre is crucial for providing integrated and patient-centered care. Opportunities exist to foster interdisciplinary education and create a culture of mutual respect and communication among healthcare professionals.
- Technological advancements: Rapid technological advancements offer opportunities for innovation and improved patient care. Challenges include ensuring that healthcare professionals are well-trained to utilize new technologies and addressing potential ethical concerns related to technology in healthcare.
- Global health threats: The emergence of global health threats, such as pandemics and infectious diseases, poses challenges in terms of preparedness, response, and international collaboration. Opportunities for global cooperation and knowledge-sharing can enhance the resilience of healthcare systems in the face of such challenges.
- Aging population: The demographic shift toward an aging population poses challenges in managing age-related health conditions, long-term care needs, and the demand for geriatric healthcare services.
Modern trends shaping healthcare

Healthcare is continually shaped by modern trends that influence the way medical services are delivered, accessed, and experienced.
From advancements in technology to shifts in patient-centric care, these trends collectively redefine the landscape of healthcare.
1. Telehealth and remote care
One of the most transformative trends in modern healthcare is the widespread adoption of telehealth and remote care solutions.
Telehealth leverages digital technologies to facilitate virtual consultations, remote monitoring, and telemedicine services.
This trend has surged, especially in response to the global pandemic, offering patients convenient access to healthcare professionals, reducing geographical barriers, and improving continuity of care.
Telehealth not only enhances accessibility but also plays a crucial role in preventive care, chronic disease management, and follow-up consultations.
2. Digital health solutions
The proliferation of digital health solutions, including mobile apps, wearable devices, and health trackers, is empowering individuals to take an active role in managing their health.
These tools enable users to monitor vital signs, track fitness, and nutrition, and receive personalized health insights.
With the integration of artificial intelligence and machine learning, digital health solutions contribute to the early detection of health issues, facilitate self-management, and promote preventive practices, fostering a more proactive and personalized approach to healthcare.
3. Precision medicine
Precision medicine represents a paradigm shift in healthcare, moving away from a one-size-fits-all model to a more personalized approach.
This trend involves tailoring medical treatment to individual characteristics, including genetic makeup, lifestyle factors, and environmental influences.
Precision medicine holds the promise of enhancing treatment efficacy, minimizing adverse effects, and optimizing therapeutic outcomes.
Advances in genomics and molecular diagnostics are driving the integration of precision medicine into clinical practice, ushering in a new era of targeted and individualized healthcare.
4. Interconnected health information systems
The seamless exchange of health information among different components of the healthcare system is a pivotal trend shaping modern healthcare.
Interconnected health information systems, facilitated by electronic health records (EHRs) and health information exchanges (HIEs), enhance care coordination, reduce medical errors, and improve the overall patient experience.
This trend ensures that healthcare professionals have access to comprehensive and up-to-date patient information, promoting collaborative and patient-centered care.
5. Patient-centered care
Patient-centered care is a transformative trend that places the patient at the center of the healthcare experience.
This approach emphasizes empathy, communication, and shared decision-making between healthcare providers and patients.
It recognizes the importance of understanding patients’ values, preferences, and individual circumstances.
Patient-centered care contributes to improved patient satisfaction, increased adherence to treatment plans, and better health outcomes, fostering a more compassionate and holistic healthcare environment.
6. Artificial intelligence (AI) and machine learning
The integration of artificial intelligence and machine learning into healthcare processes is revolutionizing diagnostics, treatment planning, and predictive analytics.
AI algorithms analyze vast datasets to identify patterns, predict disease trajectories, and assist in medical decision-making.
From image recognition in radiology to personalized treatment recommendations, AI holds the potential to augment the capabilities of healthcare professionals, reduce diagnostic errors, and enhance the efficiency of healthcare delivery.
7. Value-based care
The shift towards value-based care is a trend that redefines the traditional fee-for-service model.
Value-based care focuses on improving patient outcomes, enhancing patient experience, and controlling healthcare costs.
This approach incentivizes healthcare providers to prioritize preventive care, chronic disease management, and patient satisfaction, aligning financial incentives with positive health outcomes rather than the volume of services provided.
Conclusion
As healthcare continues to evolve, the pillars, faces, challenges, and trends within this dynamic field shape the future of how we approach well-being. Navigating the landscape of healthcare requires a commitment to patient-centered, evidence-based practices and a willingness to embrace technological advancements that enhance accessibility and quality of care. By addressing challenges, fostering collaboration, and staying attuned to emerging trends, healthcare can continue to be a beacon of hope and healing for individuals and communities worldwide.
Obisesan Damola
Damola is a medical doctor who has worked in the Nigerian healthcare industry for a little over 3 years in a number of primary, secondary, and tertiary hospitals. He is interested in and writes about how technology is helping to shape the healthcare industry. He graduated from the College of Medicine, University of Ibadan, the foremost medical training institution in Nigeria.