Hepatitis is a term used to describe inflammation of the liver, a vital organ responsible for processing nutrients, filtering toxins, and producing bile.
Hepatitis can be caused by a variety of factors, including viral infections, excessive alcohol consumption, autoimmune diseases, and exposure to certain medications or toxins.
Viral hepatitis, in particular, refers to liver inflammation caused by infection with one of several hepatitis viruses, including hepatitis A, B, C, D, and E.
These viruses differ in their modes of transmission, severity of illness, and long-term consequences.
Hepatitis infections can range from mild, self-limiting illnesses to chronic conditions that lead to progressive liver damage, cirrhosis, and liver cancer.
Despite advances in prevention and treatment, viral hepatitis remains a significant global health challenge, affecting millions of people worldwide and contributing to substantial morbidity and mortality.
Thus, understanding the causes, symptoms, prevention, and management of hepatitis is essential for effectively addressing this public health issue.
In this comprehensive guide, we’ll delve into the different types of hepatitis, their causes, symptoms, diagnosis, treatment, and prevention strategies.
The human liver
The liver is a remarkable organ that plays a vital role in maintaining overall health and well-being.
Situated in the upper right abdomen, the liver is the largest internal organ in the body and performs a multitude of essential functions.
However, the liver is also vulnerable to various diseases and conditions, including viral hepatitis, which can compromise its structure and function.
It plays a critical role in maintaining health through a wide range of essential functions.
1. Metabolic regulation
The liver acts as the body’s central processing unit for metabolism.
It breaks down carbohydrates, fats, and proteins into usable forms for energy production and tissue repair.
Additionally, it synthesizes essential molecules like glucose, cholesterol, and proteins for various bodily functions.
2. Blood detoxification
The liver acts as a natural filter, removing toxins and waste products from the bloodstream.
These can be byproducts of metabolism, environmental toxins, or medications.
The liver detoxifies these substances and prepares them for excretion through the bile or urine.
3. Bile production
The liver produces bile, a yellowish-green fluid stored in the gallbladder.
Bile aids in digestion by emulsifying fats, making them more readily available for absorption by the small intestine.
4. Blood storage and coagulation
The liver plays a vital role in maintaining blood volume by storing excess glucose as glycogen, readily available for energy when needed.
It also synthesizes clotting factors essential for proper blood clotting and wound healing.
Additionally, the liver serves as a storage center for essential nutrients like vitamins A, D, E, K, and B12.
5. Immune function
The liver plays a part in the immune system by producing immune factors and removing pathogens from the bloodstream.
Causes of hepatitis
The primary causes of hepatitis vary depending on the type:
- Viral Infections: Hepatitis A, B, C, D, and E are caused by different viruses and have distinct modes of transmission.
- Hepatitis A and E: Spread primarily through contaminated food and water.
- Hepatitis B and C: Spread through contact with infected bodily fluids like blood, semen, or vaginal fluids.
- Hepatitis D: requires the presence of hepatitis B for co-infection.
- Alcohol and drugs: Excessive alcohol consumption, certain medications, and illicit drug use can lead to toxic hepatitis.
- Autoimmune disorders: The body’s immune system mistakenly attacks the liver, leading to autoimmune hepatitis.
- Other causes: Hepatitis can also result from exposure to toxins, metabolic disorders, or certain genetic factors.
Types of viral hepatitis
There are several types of hepatitis, classified primarily as hepatitis A, B, C, D, and E, each caused by different viruses:
1. Hepatitis A
Transmitted through contaminated food, water, or close contact with an infected person.
Symptoms include fatigue, nausea, abdominal pain, jaundice, and loss of appetite.
Hepatitis A is usually acute and doesn’t result in chronic liver disease.
2. Hepatitis B
Transmitted through blood, semen, or other body fluids.
Can be acute or chronic and may lead to severe liver damage, liver cancer, or liver failure.
Symptoms may include jaundice, fatigue, abdominal pain, dark urine, and joint pain.
3. Hepatitis C
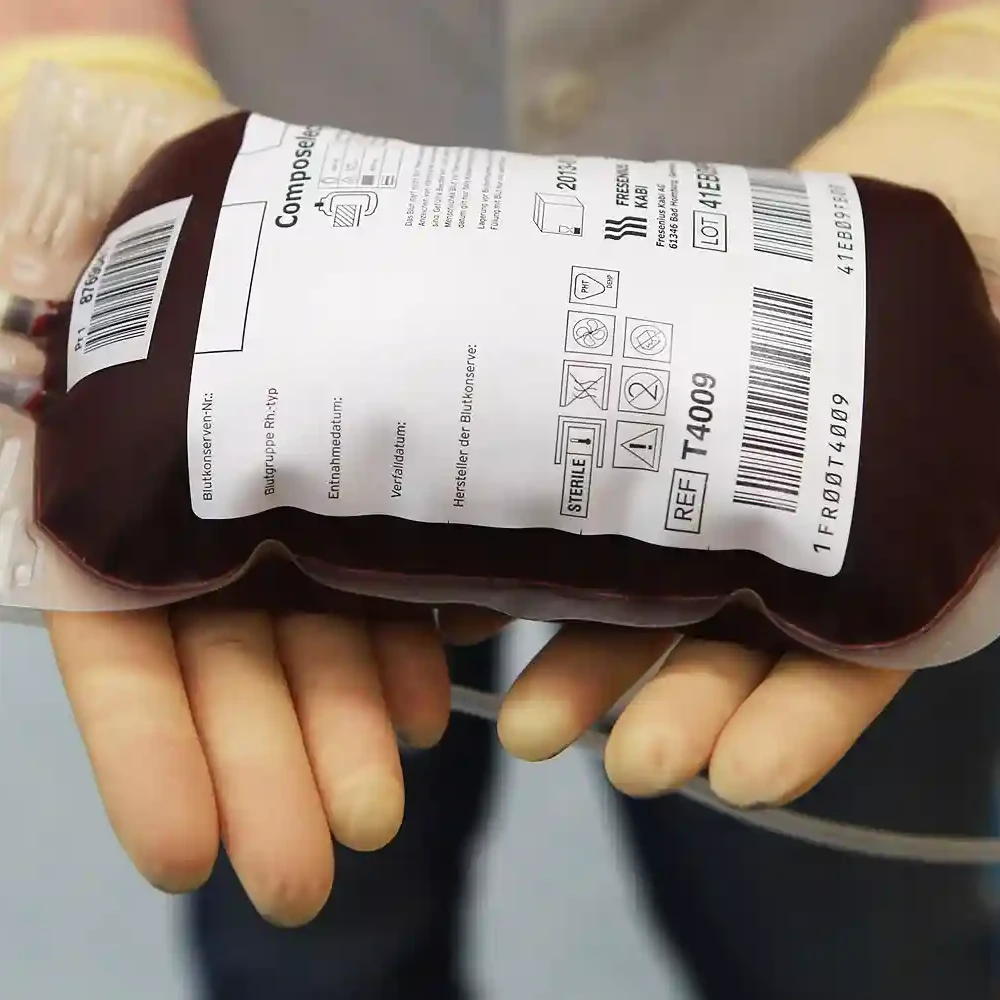
Mainly transmitted through blood-to-blood contact, such as sharing needles or receiving contaminated blood transfusions.
Often asymptomatic in the early stages, it can lead to chronic liver disease, cirrhosis, or liver cancer over time.
Symptoms may include fatigue, abdominal pain, jaundice, and joint pain.
4. Hepatitis D
It occurs only in individuals infected with the hepatitis B virus.
Transmission routes are similar to those of hepatitis B, mainly through contact with infected blood or body fluids.
Symptoms are similar to those of hepatitis B but may be more severe.
5. Hepatitis E
Typically, it spreads through contaminated water in areas with poor sanitation.
Symptoms are similar to those of hepatitis A, including fatigue, nausea, abdominal pain, and jaundice.
Hepatitis E is usually acute and self-limiting but can be severe in pregnant women.
Symptoms of hepatitis
The symptoms of hepatitis can vary depending on the type and stage of the disease.
- Jaundice (yellowing of the skin and eyes)
- Fatigue
- Nausea and vomiting
- Abdominal pain or discomfort
- Loss of appetite
- Dark urine
- Pale stools
- Joint pain
- Fever
- Enlarged liver or spleen
Diagnosis of hepatitis
Diagnosing hepatitis typically involves a combination of medical history review, physical examination, blood tests, imaging studies, and liver biopsy if necessary.
Key diagnostic tests include:
- Hepatitis serology tests are used to detect specific viral antigens and antibodies.
- Liver function tests (LFTs) are used to assess liver enzyme levels and overall liver function.
- Imaging studies such as ultrasound, CT scan, or MRI to evaluate liver structure and detect any abnormalities.
- Liver biopsy to obtain a tissue sample for microscopic examination and further evaluation of liver damage or inflammation.
Treatment and management
Treatment for hepatitis depends on the type and severity of the disease.
- Hepatitis A: usually resolves on its own without specific treatment. Rest, adequate hydration, and avoiding alcohol are recommended.
- Hepatitis B and C: Antiviral medications may be prescribed to suppress viral replication and reduce liver inflammation. In some cases, combination therapy or liver transplantation may be necessary.
- Hepatitis D and E: Treatment options are limited, and supportive care is often recommended to manage symptoms and prevent complications.
Complications of hepatitis
Hepatitis can lead to various complications that significantly impact an individual’s health and quality of life.
While hepatitis can range from mild, self-limiting illness to chronic liver disease and even liver cancer, understanding the potential complications of hepatitis is crucial for effective management and prevention.
1. Acute hepatitis
Acute hepatitis refers to short-term liver inflammation that occurs suddenly and resolves within six months.
While many cases of acute hepatitis are mild and asymptomatic, some individuals may experience symptoms such as fatigue, nausea, abdominal pain, jaundice, and dark urine.
In severe cases, acute hepatitis can progress rapidly to acute liver failure, a life-threatening condition characterized by liver dysfunction and impaired clotting function.
Acute liver failure requires urgent medical attention and may necessitate liver transplantation to prevent death.
2. Chronic hepatitis
Chronic hepatitis occurs when liver inflammation persists for more than six months, leading to ongoing liver damage and scarring (fibrosis).
Chronic hepatitis can result from persistent infection with hepatitis B or hepatitis C viruses, autoimmune hepatitis, or prolonged exposure to toxins such as alcohol or certain medications.
Over time, chronic hepatitis can progress to cirrhosis, a condition characterized by extensive liver scarring and impaired liver function.
Cirrhosis increases the risk of complications such as portal hypertension, ascites (fluid buildup in the abdomen), hepatic encephalopathy (brain dysfunction), and hepatorenal syndrome (kidney dysfunction).
3. Liver failure
Liver failure, also known as hepatic failure, occurs when the liver loses its ability to function adequately, resulting in severe impairment of metabolic, detoxification, and synthetic processes.
Acute liver failure can occur suddenly and is often precipitated by factors such as viral hepatitis, drug toxicity, or ischemic injury.
Chronic liver failure typically develops gradually over time as a result of progressive liver damage, such as that seen in advanced cirrhosis.
Liver failure can lead to a range of complications, including jaundice, coagulopathy (impaired blood clotting), hepatic encephalopathy, and multiorgan failure, ultimately culminating in death if left untreated.
4. Hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer and is closely associated with chronic liver disease, particularly cirrhosis caused by viral hepatitis or alcohol abuse.
Chronic inflammation and liver cell regeneration promote the development of HCC, which often arises in the setting of underlying liver cirrhosis.
HCC is characterized by rapid tumor growth, metastasis to other organs, and a poor prognosis, with limited treatment options and high mortality rates.
Early detection and treatment of HCC are essential for improving outcomes and prolonging survival.
Prevention strategies
Preventing hepatitis involves a combination of vaccination, adopting safe hygiene practices, and avoiding risky behaviors.
1. Vaccination
Vaccination is one of the most effective ways to prevent hepatitis, particularly hepatitis A and hepatitis B.
The hepatitis A vaccine provides immunity against the hepatitis A virus and is recommended for individuals traveling to endemic areas, men who have sex with men, and individuals at increased risk of exposure to the virus.
Similarly, the hepatitis B vaccine protects against hepatitis B virus infection and is routinely administered to infants, healthcare workers, and individuals at high risk of HBV transmission, such as injection drug users and those with multiple sexual partners.
Ensuring that individuals receive the recommended vaccinations and completing the full vaccine series is essential for long-term protection against hepatitis.
2. Practice good hygiene
Practicing good hygiene is crucial for preventing the spread of hepatitis viruses, particularly hepatitis A and E, which are primarily transmitted through contaminated food or water.
Individuals should wash their hands thoroughly with soap and water after using the bathroom, before preparing or eating food, and after handling potentially contaminated objects or surfaces.
Additionally, avoiding the consumption of raw or undercooked shellfish, practicing safe food handling and preparation techniques, and drinking safe, clean water from a reliable source can help reduce the risk of hepatitis A and E infection.
3. Practice safe sex
Practicing safe sex is important for preventing the transmission of hepatitis B and hepatitis C, which can be spread through sexual contact with an infected individual.
Using condoms consistently and correctly during sexual intercourse can help reduce the risk of HBV and HCV transmission.
Individuals should also limit their number of sexual partners and avoid sharing needles or other equipment used for injecting drugs, tattooing, or body piercing, as these activities can increase the risk of hepatitis transmission.
4. Avoid sharing personal items
Avoiding the sharing of personal items that may come into contact with blood or bodily fluids is essential for preventing hepatitis B and hepatitis C transmission.
Individuals should refrain from sharing razors, toothbrushes, needles, syringes, or other personal care items that may be contaminated with blood.
Ensuring that medical and dental equipment is properly sterilized and disposable needles and syringes are used for medical procedures and injections can also help prevent hepatitis transmission in healthcare settings.
5. Get tested and seek treatment
Regular testing for hepatitis B and hepatitis C is important for identifying infections early and initiating appropriate treatment to prevent disease progression and transmission.
Individuals at increased risk of hepatitis infection, such as healthcare workers, people living with HIV, injection drug users, and individuals born to HBV-infected mothers, should undergo screening for hepatitis as part of routine medical care.
If diagnosed with hepatitis, individuals should seek medical evaluation and follow-up care to monitor liver health and discuss treatment options, including antiviral medications, lifestyle modifications, and liver transplantation when indicated.
Hepatitis vaccines

Hepatitis vaccines are immunizations designed to protect against viral infections that primarily affect the liver, namely hepatitis A and hepatitis B.
These vaccines work by stimulating the body’s immune system to produce antibodies against the respective hepatitis viruses, thereby providing immunity and preventing infection.
Both vaccines are highly effective in preventing hepatitis A and hepatitis B infections and have been instrumental in reducing the global burden of these diseases.
The importance of hepatitis vaccines
Hepatitis vaccines offer numerous benefits to individuals and communities.
- Prevention of liver disease: Hepatitis vaccines prevent acute and chronic liver diseases caused by hepatitis viruses, reducing the burden on healthcare systems and improving overall public health.
- Protection against complications: Vaccination protects against severe complications of hepatitis infections, including liver failure, cirrhosis, and liver cancer.
- Herd immunity: High vaccination coverage within communities can lead to herd immunity, reducing the transmission of hepatitis viruses and protecting vulnerable populations.
- Cost-effective intervention: Vaccination is a cost-effective public health intervention, with the long-term benefits outweighing the costs associated with treating hepatitis-related illnesses.
Types of hepatitis vaccines
There are vaccines available for hepatitis A and hepatitis B, offering protection against these viral infections.
Let’s explore each vaccine in detail:
1. Hepatitis A Vaccine:
The hepatitis A vaccine protects against the hepatitis A virus (HAV), which is primarily transmitted through contaminated food and water or close contact with an infected person.
The vaccine contains inactivated HAV, stimulating the immune system to produce antibodies against the virus, thus providing immunity.
Hepatitis A vaccines are highly effective and typically administered in two doses, with the second dose given 6 to 12 months after the first dose.
2. Hepatitis B Vaccine:
The hepatitis B vaccine protects against the hepatitis B virus (HBV), which is transmitted through blood, semen, or other body fluids.
The vaccine contains a recombinant HBV surface antigen (HBsAg), which triggers the production of antibodies that neutralize the virus.
Hepatitis B vaccination is usually administered as a series of three or four doses, depending on the vaccine formulation and schedule.
Who should get vaccinated?
The vaccination against hepatitis is recommended for:
- Infants and children: Routine vaccination against hepatitis A and hepatitis B is recommended as part of childhood immunization schedules in many countries.
- Adults: Vaccination is recommended for individuals at increased risk of hepatitis infection, including travelers to endemic areas, healthcare workers, injection drug users, and individuals with certain medical conditions.
- High-risk populations: Special consideration should be given to populations at higher risk of hepatitis infection or its complications, including men who have sex with men, individuals with chronic liver disease, and pregnant women at risk of perinatal HBV transmission.
World Hepatitis Day
World Hepatitis Day is observed annually on July 28th to raise awareness about viral hepatitis, promote prevention measures, and advocate for improved access to testing, treatment, and care for those affected by hepatitis.
The day serves as a global platform for individuals, organizations, and governments to come together and address the challenges posed by hepatitis, including its significant impact on public health and well-being.
Through various activities and initiatives, such as educational campaigns, community outreach events, free testing and vaccination drives, policy advocacy efforts, and fundraising activities, World Hepatitis Day aims to mobilize action against hepatitis and accelerate progress towards the elimination of viral hepatitis as a major public health threat.
Conclusion
Hepatitis is a significant public health concern worldwide, with various types posing significant risks to liver health and overall well-being.
Understanding the different types, causes, symptoms, and prevention strategies is essential for effective management and prevention.
By promoting vaccination, practicing good hygiene, and adopting safe behaviors, individuals can reduce their risk of hepatitis and safeguard their liver health for a healthier future.
If you suspect you may have hepatitis or are at risk, consult a healthcare professional for proper evaluation and management.
Damola Obisesan
Damola is a medical doctor who has worked in the Nigerian healthcare industry for a little over 3 years in a number of primary, secondary, and tertiary hospitals. He is interested in and writes about how technology is helping to shape the healthcare industry. He graduated from the College of Medicine, University of Ibadan, the foremost medical training institution in Nigeria.