In medicine, making diagnoses of diseases and medical conditions depends on a delicate balance of evidence and educated guesswork.
A battery of tests serves as detective work, unearthing the culprits behind our ailments.
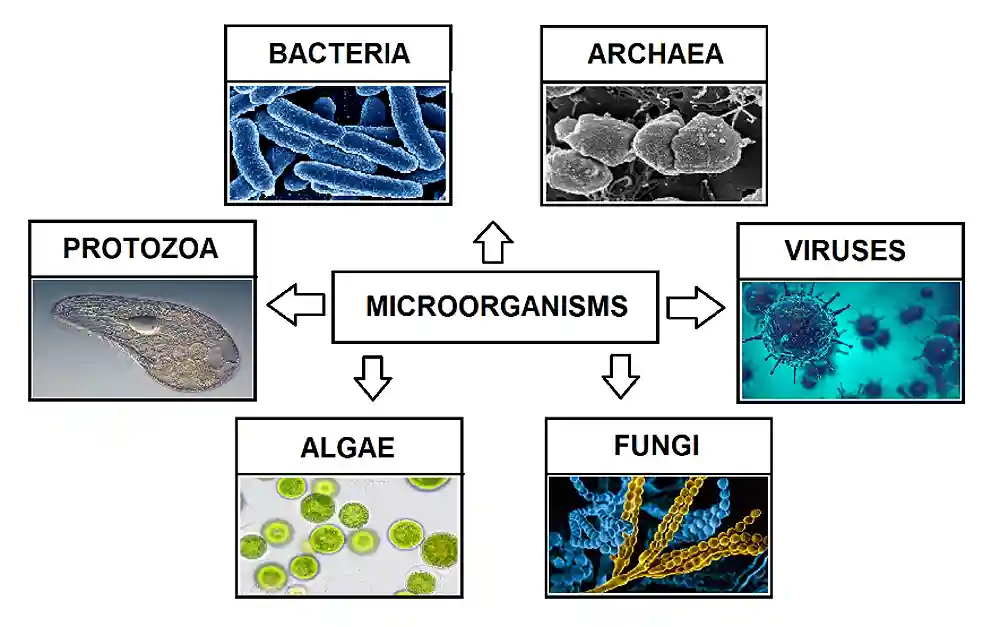
Among these investigative tools, microscopy, culture, and sensitivity testing (MCS) stand as a potent trio, offering invaluable insights into the microbial world lurking within our bodies.
The test stands as a formidable tool for unraveling the mysteries of infectious diseases.
This blog post delves into the intricacies of MCS, exploring its components, applications, and the pivotal role it plays in guiding precise and effective medical interventions.
Microscopy, culture, and sensitivity (MCS)
The Microscopy, Culture, and Sensitivity (MCS) test is a comprehensive diagnostic approach in medicine that plays a pivotal role in identifying and characterizing infectious agents and guiding precise treatment strategies.
The information obtained from the MCS test is instrumental in guiding healthcare providers in selecting the most effective and targeted antimicrobial therapy for individual patients.
This approach not only aids in the accurate diagnosis of infectious diseases but also ensures that treatment plans are tailored to the specific characteristics of the identified pathogens, minimizing the risk of treatment failure and the development of antimicrobial resistance.
The MCS test is widely used in infectious disease management, providing valuable insights for clinicians to make informed decisions about patient care.
Samples used for MCS
Microscopy, culture, and sensitivity testing are used in evaluating various clinical scenarios, including:
- Wound swab (in wound infections)
- Throat swab or sputum sample (in respiratory infections)
- Skin sample (in skin infections)
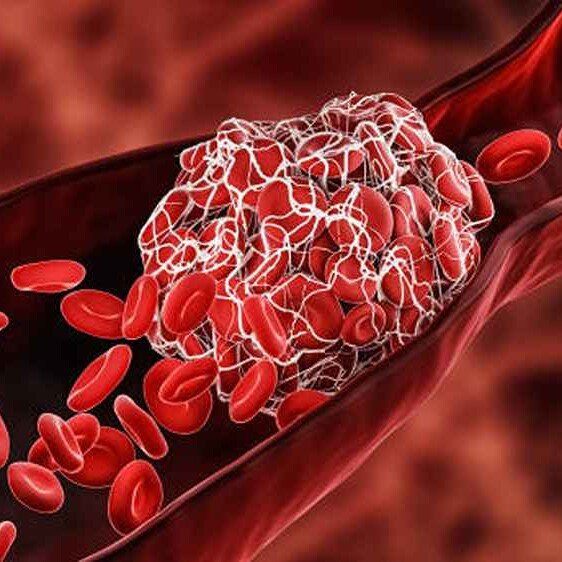
- Blood sample (in bloodstream infections)
- Cerebrospinal fluid sample (in CNS infections)
- Urine sample (in urinary tract infections)
- Etc.
The MCS workflow
- Sample collection: The MCS journey begins with the collection of clinical specimens, such as blood, urine, sputum, or tissue samples, depending on the suspected infection site.
- Microscopic examination: Microscopy allows for the direct observation of cellular structures or pathogens in the clinical sample, providing initial clues about the nature of the infection.
- Culturing process: Clinical specimens are inoculated onto specific culture media, fostering the growth of microorganisms. The resulting colonies are then isolated for further characterization.
- Identification: Once isolated, the cultured microorganisms are identified using various techniques, including biochemical tests, mass spectrometry, or molecular methods, depending on the laboratory’s capabilities.
- Sensitivity testing: The identified pathogens undergo sensitivity testing, assessing their response to a panel of antimicrobial agents. This step informs healthcare providers about the most appropriate and effective treatment options.
- Clinical decision-making: Armed with the comprehensive information obtained through MCS, healthcare professionals can make informed decisions regarding the choice of antimicrobial therapy, dosage, and duration, tailored to the specific characteristics of the identified pathogens.
Microscopy
Microscopy, the first component of MCS, provides a lens through which medical professionals can peer into the microscopic world.
Employing various techniques, such as light microscopy, electron microscopy, or fluorescence microscopy, healthcare practitioners can visualize microorganisms, cells, or cellular structures.
Tiny snippets of tissue or fluids suspected of harboring microbial mischief are stained and magnified, revealing a landscape teeming with microscopic characters.
Bacteria, with their diverse shapes and arrangements, take center stage, their presence and morphology offering the first clues to the identity of the potential pathogen.
This allows for the direct observation of pathogens in clinical samples, their rapid identification, and preliminary insights into the nature of infections.
While not definitive, a skilled microbiologist can glean valuable information from this microscopic stage play, narrowing down the suspects and directing the investigation further.
Culture
Culture, the second component of MCS, involves the cultivation of microorganisms in a controlled environment.
By providing optimal conditions for growth, healthcare professionals can isolate and propagate pathogens obtained from clinical specimens.
Enriched broths and agar plates, like gourmet platters for microscopic guests, provide the perfect environment for them to multiply and reveal their true colors.
Throughout incubation, the broth may cloud, or colonies may sprout on the agar, each a miniature city of the offending microbe.
The culturing process allows for the identification of specific microorganisms, facilitating a deeper understanding of their characteristics, behaviors, and potential susceptibilities to antimicrobial agents.
This cultivation process acts as a confirmation step, providing definitive proof of the presence of the suspected pathogen.
Additionally, the specific type of media used and the growth patterns observed offer further clues about the microbe’s identity and preferences, aiding in pinpointing the exact culprit.
Sensitivity
The third component, sensitivity, completes the MCS triumvirate by evaluating how microorganisms respond to various antimicrobial agents.
Sensitivity testing involves exposing cultured microorganisms to different antibiotics, antifungals, or antivirals and assessing their responsiveness.
This stage assesses the offending organism’s susceptibility to an arsenal of antibiotics.
Different antibiotics are strategically placed on the agar plate, creating a battlefield where their effectiveness is tested.
Clear zones around an antibiotic disc signify the microbe’s surrender and its inability to grow in the presence of that particular weapon.
This information is crucial for guiding the choice of antibiotic therapy and ensuring the most effective and targeted attack against the foe.
This critical step guides healthcare providers in determining the most effective treatment options, ensuring that prescribed medications target the identified pathogens with optimal precision.
Applications of MCS in medicine
- Infectious disease diagnosis: MCS is instrumental in diagnosing various infectious diseases, including bacterial, fungal, and parasitic infections, by identifying the causative agents. Identifying the specific bacterial strain provides valuable information about its antibiotic resistance patterns, ensuring targeted and effective treatment.
- Treatment guidance: Sensitivity testing guides healthcare providers in selecting antimicrobial agents that are most effective against the identified pathogens, minimizing the risk of treatment failure and the development of antimicrobial resistance.
- Monitoring treatment efficacy: Periodic MCS assessments allow healthcare professionals to monitor the progress of treatment and make adjustments if necessary, ensuring a targeted and responsive approach to managing infections.
- Outbreak investigations: In the context of outbreaks or nosocomial infections, MCS plays a crucial role in identifying the source of infection and implementing appropriate control measures.
- Differentiating infection from inflammation: Not all symptoms point to an infection. This test helps distinguish a true bacterial infection from other causes of similar symptoms, like inflammation or irritation.
Conclusion
While seemingly complex, microscopy, culture, and sensitivity testing play a crucial role in the accurate diagnosis and targeted treatment of infections.
This three-pronged approach helps to identify the causative agent, determine its susceptibility to antibiotics, and ultimately guide physicians in choosing the most effective course of action for optimal patient outcomes.
As we navigate the landscape of infectious diseases, MCS remains a cornerstone in our collective defense, safeguarding our health and well-being, one microscopic clue at a time.
Obisesan Damola
Damola is a medical doctor who has worked in the Nigerian healthcare industry for a little over 3 years in a number of primary, secondary, and tertiary hospitals. He is interested in and writes about how technology is helping to shape the healthcare industry. He graduated from the College of Medicine, University of Ibadan, the foremost medical training institution in Nigeria.