Semen analysis is a crucial diagnostic tool used to evaluate male fertility potential.
It provides valuable insights into various parameters of semen quality, aiding in the assessment of reproductive health.
In this article, we will discuss the details of semen analysis, its significance, the procedure involved, and what the results indicate.
What is semen analysis?
The journey to parenthood can be a thrilling yet complex one.
For couples struggling with conception, a range of factors can contribute to infertility.
Semen analysis, a cornerstone of male fertility evaluation, offers a valuable window into a man’s reproductive potential.
This non-invasive test analyzes various aspects of semen, providing crucial information for both diagnosis and treatment planning.
Semen analysis, also known as a sperm count test, is a laboratory examination of semen to assess its quality and quantity.
It involves evaluating several parameters, including sperm count, motility, morphology, volume, pH level, and the presence of any abnormalities or infections.
The significance of semen analysis
The significance of semen analysis lies in its ability to provide valuable insights into male reproductive health and fertility potential.
Here are some key implications of semen analysis:
- Assessment of male fertility: Semen analysis is a primary diagnostic tool used to assess male fertility. By evaluating parameters such as sperm count, motility, and morphology, healthcare providers can determine the likelihood of successful fertilization and conception.
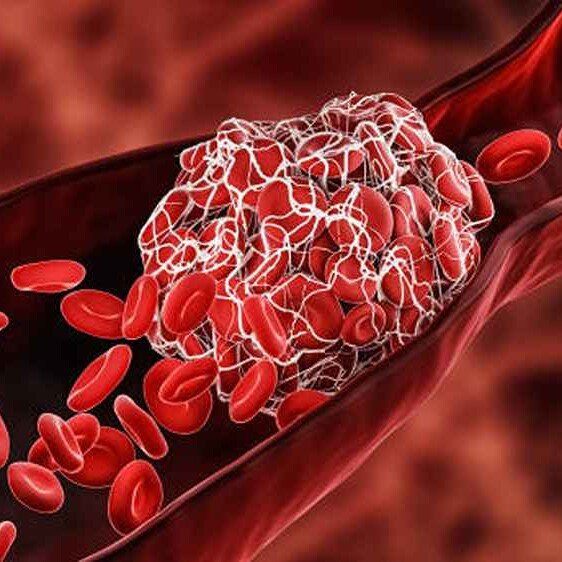
- Identification of fertility issues: Abnormalities in semen parameters detected through analysis can indicate underlying fertility issues. Low sperm count (oligospermia), poor sperm motility (asthenospermia), or abnormal sperm morphology (teratospermia) may hinder the ability to achieve pregnancy naturally.
- Guidance for treatment options: Semen analysis results help healthcare providers tailor treatment strategies for couples struggling with infertility. Depending on the findings, treatment options such as lifestyle modifications, medications, or assisted reproductive techniques like in vitro fertilization (IVF) or intrauterine insemination (IUI) may be recommended.
- Monitoring treatment progress: For individuals undergoing fertility treatments, semen analysis serves as a tool for monitoring treatment efficacy and progress. Regular analysis of semen parameters allows healthcare providers to adjust treatment protocols as needed to optimize outcomes.
- Preventive screening for reproductive health issues: Semen analysis may also be performed as a routine screening test for men seeking to assess their reproductive health. Early detection of abnormalities or suboptimal semen parameters can prompt interventions to address underlying conditions and prevent future fertility problems.
- Evaluation of overall health: Changes in semen quality may sometimes reflect underlying health issues beyond fertility concerns. Semen analysis results can provide insights into overall health, highlighting potential systemic conditions or lifestyle factors that may impact reproductive function.
- Preconception counseling: Semen analysis is often recommended as part of preconception counseling for couples planning to conceive. It allows healthcare providers to identify any potential barriers to fertility and provide guidance on optimizing reproductive health before attempting to conceive.
- Research and advancements in reproductive medicine: Semen analysis data contributes to ongoing research in reproductive medicine, leading to advancements in understanding male infertility and developing innovative treatments.
How is semen analysis done?
The process of semen analysis typically begins with collecting a semen sample through ejaculation into a sterile container provided by the healthcare provider.
1. Preparation before scheduling a semen analysis
It is essential to follow specific guidelines provided by your healthcare provider:
- Abstain from ejaculation for 2 to 5 days before the test. This ensures that the semen sample contains an adequate number of sperm for analysis.
- Avoid substances that may interfere with semen quality, such as lubricants, spermicides, or medications not prescribed by your healthcare provider.
- Collect a sterile container from the healthcare facility where you will undergo the semen analysis.
2. Collection of semen sample
Semen samples are typically collected through masturbation into a sterile container provided by the healthcare provider.
It’s crucial to collect the entire ejaculate to ensure an accurate analysis.
- Find a private and comfortable place where you can ejaculate without interruption.
- Wash your hands thoroughly with soap and warm water before collecting the sample to prevent contamination.
- Masturbate into the sterile container provided, ensuring that the entire ejaculate is collected.
3. Transporting the semen sample
Once the semen sample is collected, it should be transported to the laboratory for analysis as soon as possible.
Follow these guidelines to ensure the integrity of the sample:
- Keep the sample container tightly closed to prevent leakage or contamination.
- Transport the sample to the laboratory within the specified time frame provided by your healthcare provider.
In most cases, semen samples should be analyzed within one hour of collection to obtain accurate results.
4. Laboratory analysis
Upon receiving the semen sample, trained laboratory technicians perform a comprehensive analysis to evaluate various parameters of semen quality.
The analysis typically includes the following steps:
- Semen volume: The volume of the ejaculate is measured to determine the quantity of semen produced.
- Sperm count: Using a specialized microscope, technicians count the number of sperm present in a specific volume of semen.
- Sperm motility: Technicians assess the percentage of sperm that exhibit forward movement (motility), which is crucial for sperm to reach and fertilize the egg.
- Sperm morphology: The size and shape of sperm are examined to identify abnormalities that may affect fertility.
- Semen pH: The acidity or alkalinity of the semen is determined to assess its physiological properties.
- Abnormalities or infections: Semen analysis also includes the examination for the presence of white blood cells, which may indicate infection, as well as any other abnormalities or debris.
5. Interpretation of results
Once the semen analysis is complete, the results are interpreted by a healthcare provider.
Depending on the findings, further evaluation or treatment may be recommended to address any identified issues affecting male fertility.
Interpretation of semen analysis results
The results of semen analysis provide valuable information about male fertility potential.
Here’s what each parameter indicates:
- Sperm count: This refers to the number of sperm present in one milliliter of semen. A normal sperm count typically ranges from 15 million to 200 million sperm per milliliter. A low sperm count (oligospermia) may indicate fertility issues.
- Sperm motility: It measures the percentage of sperm that are moving actively. Motility is crucial for sperm to reach and fertilize the egg. Normal sperm motility is typically greater than 40%. Reduced motility (asthenospermia) can hinder the sperm’s ability to reach the egg.
- Sperm morphology: Morphology assesses the size and shape of sperm. Normal morphology indicates that a significant percentage of sperm have a typical shape, which is essential for successful fertilization. Abnormal morphology (teratospermia) may affect the sperm’s ability to penetrate the egg.
- Semen volume: It measures the amount of semen ejaculated. Normal semen volume ranges from 1.5 to 6 milliliters. Low semen volume may indicate issues with sperm production or ejaculatory duct obstruction.
- pH level: semen pH reflects the acidity or alkalinity of the semen. Normal pH levels range from 7.2 to 8.0. Deviations from this range may indicate infections or other underlying conditions.
- Presence of abnormalities or infections: Semen analysis also checks for the presence of white blood cells, which may indicate infection, as well as any other abnormalities such as clumping of sperm or the presence of debris.
Obisesan Damola
Damola is a medical doctor who has worked in the Nigerian healthcare industry for a little over 3 years in a number of primary, secondary, and tertiary hospitals. He is interested in and writes about how technology is helping to shape the healthcare industry. He graduated from the College of Medicine, University of Ibadan, the foremost medical training institution in Nigeria.